Abstract
Introduction
The novel pediatric-like and TKI-based induction regimens induce up to 90 % of complete hematologic response in, respectively, Ph'-negative and Ph'-positive B-Cell Acute Lymphoblastic Leukemia (B-ALL). Minimal residual disease (MRD) strongly correlates with relapse and clearance of MRD is the goal of treatment.
Blinatumomab is a bispecific T-cell engager that redirects T-Cells to kill CD19+ cells. Data from clinical trials show that the MRD-positive patients responding to Blinatumomab achieve a better survival than the non-responsive.
This retrospective study from real-life demonstrates a superior outcome for MRD-responsive patients to blinatumomab over non-responsive patients.
Patients and methods
Data from adults treated with blinatumomab in six centers were analyzed to identify factors correlated to survival. Each cycle of blinatumomab was administered in 4 weeks at 15 mg/m2/day by continuous infusion followed by a 2-week interval. Intrathecal prophylaxis with ARA-C, Methotrexate and Dexamethasone was performed between cycles. Twenty-nine (87 %) patients received levetiracetam for seizure-prophylaxis.
MRD was measured after each cycle by RT-qPCR with a sensitivity of 10-4 for clonal IgH and for BCR-ABL.
As MRD response was considered clonal IgH or BCR-ABL < 10-4.
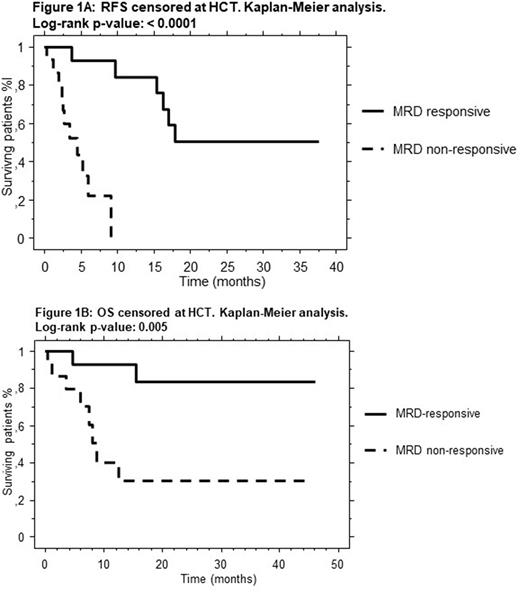
Relapse-free survival (RFS) and overall survival (OS) were estimated by the Kaplan-Meier analysis and compared by the log-rank across the sub-groups using 95 % confidence intervals. The significant variables were compared in multivariate analysis by the log-logistic regression model.
Toxicity was graded according to CTCAEs v.4 scale.
Results
From January 2016 to February 2021 34 B-ALL patients received Blinatumomab. The median age was 37 (18-72). Male to female ratio was 14/20. B-ALL was Ph'+ in 9 and Ph'- in 25 patients, respectively.
Indications to blinatumomab were, respectively, relapsed/refractory B-ALL in 19 and MRD-positive in 15 patients. SNC disease was negative before blinatumomab in all patients. Blinatumomab was administered, respectively, as 2nd line in 26 and as > 2nd line of therapy in 8 patients. Overall, 24 patients received hematopoietic transplantation (HCT): 10 before and 14 after blinatumomab, respectively.
The cycles of blinatumomab were 1, 2, 3 and 4, respectively, in 10, 13, 5, and 5 patients.
The response to blinatumomab was, respectively, complete remission without MRD in 17 (50 %), complete remission with MRD in 8 (23 %), refractory in 4 (12 %) and extramedullary progression in 2 (6 %) patients. Three patients (9 %) had to suspend treatment in 1st cycle because of grade III-IV neuro-toxicity. The response was obtained after 1 and 2 cycles in 18 (72 %) and 7 patients (28 %), respectively. Among the MRD-responsive, MRD-negativity was obtained after 1 and 2 cycles in 16 (93 %) and 1 (7 %) patient, respectively.
At a median follow-up of 16 months (1-47) 15 patients (44 %) had relapsed, 15 (44 %) were alive and in complete remission and 4 (12 %) died of transplant-related mortality. The median RFS was 12.5 months (1-39). The median OS was 15.5 months (1-46).
The median RFS was 21 vs 4.4 months among MRD-responsive and non-responsive patients, respectively (p = .0004). The median OS was 27 vs 8.7 months among MRD-responsive and non-responsive patients, respectively (p = .008).
Apart from MRD-response, the other variables significant for RFS were: blinatumomab as ≤ 2nd line (p = .0008), blinatumomab administered pre-HCT (p = .002) and MRD as an indication to treatment (p = .001). Apart from MRD-response, the other variable significant for OS was MRD as an indication (p = .01).
By multivariate analysis only the MRD-response resulted significant for RFS (p = .0009) and OS (p = .02).
MRD-response resulted significantly for RFS and OS also by censoring at HCT (p < .0001 and .005, respectively) [Figure 1].
Clinically significant toxicity was: grade II cytokine-release syndrome in 2 patients, grade III and IV neuro-toxicity in 2 and 1 patient, respectively. Overall, the percentage of patients experiencing grade III-IV neuro-toxicity, which occurred in 1st cycle, was 9 %.
Conclusion This retrospective study in adult B-ALL Ph'- and Ph'+ patients, confirms the ability of blinatumomab to reach the MRD-negativity in a substantial proportion of patients. MRD-responsive gain a significant survival advantage over non-responsive patients. This advantage was observed both for transplanted and non-transplanted patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal